
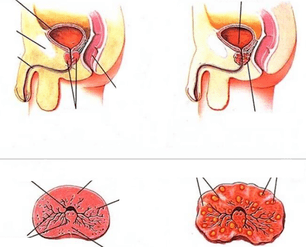
Chronic prostatitis is an inflammatory disease characterized by lesions of the prostate and severe urodynamic disorders. One of the causes of chronic inflammation of the prostate is improper or premature treatment in the acute stage, when the desquamation and proliferation of the glandular epithelium is reversible and successfully corrected by medication within 2-3 weeks.
Treatment of chronic prostatitis includes massive antibiotic therapy to eradicate the infectious agent, a number of measures to increase the body's immune resistance, physiotherapy methods and thermotherapy. Psychocorrection can also be included in the therapy regimen, since neurasthenic and neurosis-like conditions are often observed in men with long-term and recurrent prostatitis.
Why does inflammation become chronic?
The causes of chronic inflammation of the prostate must be known in order to prevent exacerbations and improve the patient's quality of life. There are a large number of factors that affect the functional state of the glandular tissue of the prostate and can cause its inflammation, which is based on the desquamation and proliferation of epithelial cells.
The main cause of chronic prostatitis in men is the extensive contamination of the mucous membranes of the urogenital system by pathogenic microorganisms. In the vast majority of cases (more than 80%) of infectious prostatitis, gram-negative and gram-positive bacteria become the causative agent of the infection: enterobacteria (especially Escherichia coli), gonococci, staphylococci. Less often, the infectious and inflammatory process proceeds against the background of infection with viruses, fungi and protozoa. However, such forms of prostatitis are treated quite successfully during the acute phase and rarely lead to relapses if treated correctly and in a timely manner.
It should also be taken into account that a single acute urinary tract infection is sufficient for the development of chronic aseptic prostatitis. Therefore, personal hygiene, the use of condoms during sexual intercourse and the timely treatment of diseases of the urinary tract are of great importance in the prevention of this disease in men. Medicine knows cases of hematogenic (through the systemic circulation) infection of the prostate in chronic sinusitis, tonsillitis and other diseases that contribute to the active growth of pathogenic flora. Therefore, the rehabilitation of chronic foci of infection is an important stage in the complex treatment of persistent or protracted inflammation of the prostate.
Negative factors that can cause prostatitis to worsen (including its non-infectious course) are:
- Urinary tract injuries and operations on the organs of the genitourinary system;
- regular or severe hypothermia of the pelvic organs (swimming in open water at times when the water is not sufficiently heated or the weather is cool outside, working in refrigerators and freezers, etc. );
- hypodynamia from sedentary work and insufficient physical activity of a man (a sedentary lifestyle is one of the main factors in the development of chronic cognitive prostatitis);
- bad habits, in which the absorption of the main macro and micro elements that determine the chemical composition and rheological properties of prostate secretions (zinc, chromium, selenium, manganese) is slowed down or impaired;
- disorders in the intimate area (frequent masturbation, irregular sexual relations, long periods of abstinence, frequent arousal that does not end with sexual intercourse);
- overweight;
- Eating disorder (increased consumption of spicy, too salty, smoked and fatty foods).
watch out! Urologists note that the main pathogenetic factor in the development of chronic inflammation of the prostate is posterior urethritis. Inflammatory changes in the prostate in men have also been found to occur in the first few months after gonorrhea infection.
Treatment of chronic prostatitis with medication
Drug treatment of chronic prostatitis is aimed only at suppressing acute symptoms during exacerbation and destruction of the infection. However, drugs cannot be used as the only means (the effectiveness of such treatment, according to Dr. Pechersky, will not exceed 36%).
The following table provides a complete drug treatment regimen for protracted or recurrent prostate inflammation that is now used as the standard for uncomplicated diseases.
table. Preparations for the complex treatment of chronic prostatitis.
| Pharmacological group | Purpose |
|---|---|
| Antibiotics from the group of macrolides, semi-synthetic penicillins and cephalosporins of the third generation with a broad spectrum of antibacterial activity. | Extermination (destruction) of pathogenic bacteria - causative agents of infectious prostatitis, urethritis, cystitis and other urinary tract infections. |
| Antimicrobial and antiprotozoal agents. | Treatment of infections caused by pathogenic microbes and protozoa. |
| Non-steroidal anti-inflammatory drugs (preferably in the form of rectal suppositories). | Reduction of the inflammatory process in the tissue of the prostate, relief of pain in the perineum, intergluteal space, sacrum and groin. |
| Antiseptics in the form of rectal suppositories. | Rehabilitation of the rectal mucous membranes and prevention of their infection with prolonged prostatitis. |
| Alpha blockers. | normalization of urination, restoration of daily urine output. |
| Microcirculation correctors. | Removal of congestion in the vessels of the pelvis, restoration of normal blood and lymph flow |
| Corrections of urodynamics (active ingredients that influence the metabolism in the tissues of the prostate). | Improvement of the metabolic and metabolic processes in the tissue of the prostate and its nutrition. |
| Power regulators. | Complex treatment of erectile dysfunction, improving the chemical composition, viscosity and fluidity of semen, increasing sperm activity (the use of drugs of this group is indicated for patients with prostatitis, complicated by autoimmune infertility). |

The duration of the antibiotic treatment is at least 4-6 weeks. In no case should you take antibacterial drugs without a doctor's prescription, since the most important factor in choosing therapy will be the results of a microscopic examination of the secretion of the prostate and the fluids spontaneously released by prostate massage. Some antibiotics, for example, penicillins (a combination of amoxicillin with clavulanic acid), are reserve drugs, and their incorrect use can lead not only to the lack of a clinically significant effect and the progression of pathology, but also to the development of superinfection.
Important! In some cases, men with chronic prostatitis need psycho-correction, especially when the pain syndrome is combined with behavioral changes, increased anxiety, irritability, and neurasthenia. Antidepressants with selective serotonin reuptake inhibition are used to suppress these symptoms.
Physiotherapy
Heat therapy is the main method of treating chronic prostatitis outside of periods of exacerbation (after regression of acute symptoms). Heat therapy refers to the methods of physiotherapy and is a metered effect of heat on the affected area. The advantages of thermal interventions lie in normalizing blood circulation, relieving inflammatory processes and reducing chronic pelvic pain, which is one of the main clinical manifestations of chronic prostatitis and affects men's quality of life. Heat also improves the penetration of drugs into the prostate tissue. Therefore, in some cases, physical therapy is used to increase the effectiveness of drug therapy (e. g. , electrophoresis with antibiotics). In men at high risk of thrombus formation, warming is prescribed for prophylaxis, since heat has a moderate absorbent effect.
There are a variety of methods of thermal action on the body, and the selection of a specific method of treatment should be carried out by a doctor, taking into account the clinical picture, the form and stage of the disease, the age of the man and his individual tolerance. The most effective methods of heat therapy for prostatitis are:

- thermal applications with minerals (ozokerite, paraffin, bishopite), salt or sand;
- electric heating pads;
- deep heating of high-strength tissue for a direct effect on blood vessels and nerve endings (diathermy);
- Exposure to high-frequency alternating magnetic fields for the elimination of pain, for the relief of inflammation and for the elimination of neurosis-like manifestations (inductothermia);
- Ultrasound therapy (promotes the absorption of abscesses and the healing of scars that have formed);
- electrophoresis with the introduction of electrodes into the rectum;
- Exposure to the prostate tissue through high-frequency impulse currents (darsonvalization).
In some physiotherapy rooms, chronic inflammation of the prostate is treated with hot mud applications ("mud pants"). Such procedures have a positive effect not only on blood circulation and lymph, but also on the production of prostate secretions, as well as on the tissue nutrition of the inflamed organ. In some cases, mud in the form of tampons is injected directly into the rectum, since this method of administration can quickly achieve a therapeutic effect and a positive response to therapy.
Other treatments
The scheme of complex treatment, in addition to drug and heat therapy, is supplemented by various procedures prescribed by the doctor, each taking into account the peculiarities of the pathology.
prostate massage
This is one of the main methods of treating chronic inflammation of the prostate, recommended in almost 90% of cases (with no contraindications). Massage is a finger effect on the prostate to stimulate the outflow of secretion fluid. The procedure usually takes about 1-2 minutes. The criterion for a sufficient effect is the complete emptying of the prostate, which the patient feels as a relief (about which he should inform the doctor).
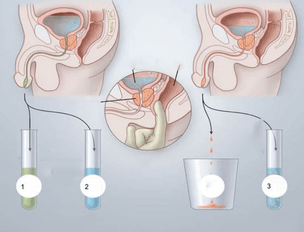
The benefits of massage are determined by the therapeutic effect that can be achieved after one treatment (8-12 procedures). For an uncomplicated course, these are:
- normalization of muscle tone;
- Improvement of blood circulation in the vessels of the prostate (this accelerates the transport of drugs into the tissues of the affected organ and increases the effectiveness of therapy);
- restoration of the secretory patency;
- Normalization of the outflow of blood and lymph from the prostate (especially significant in cognitive prostatitis).
The procedure is contraindicated during the acute phase due to the high risk of the infection spreading to surrounding tissues and organs (hematogenous infection), with other infectious diseases of the genitourinary system, the presence of cysts or stones in the prostate. Massage of the prostate is not prescribed in patients diagnosed with tuberculous organ damage, adenoma, or other neoplastic diseases (including cancerous lesions of the prostate). For rectal diseases (hemorrhoids, anal fissures, proctitis, paraproctitis), massage can cause complications and cause the underlying disease to relapse.
Important! Studies show that almost 42% of men refuse prostate massage due to the increased psychological discomfort associated with the specifics of this procedure. The doctor's work with such patients should include detailed information about the consequences of refusing treatment and possible complications, especially infertility and persistent sexual dysfunction. In some cases it may be advisable to prescribe light sedatives a few days before starting treatment.
Hot enemas
Hot enemas are home treatments for chronic prostatitis, but urologists recognize their effectiveness and recommend them for faster, more effective prostatitis treatment. The water temperature for these enemas should be 42 ° C. Before the procedure, it is necessary to clean the intestines with a regular enema or laxatives. The volume of an enema is 150-300 ml. It is recommended to empty the bowel 30-50 minutes after the administration of the solution.

The recipes for chronic prostate inflammation are listed below.
- Dissolve 10 drops of iodine and about 20 ml of chlorhexidine in 200 ml of water. Apply 15 days before bedtime.
- A brew of chamomile, St. John's wort or marigold should be introduced into the rectum (approx. 250 ml) and then kept for 1 hour. The process is repeated once a day for 2 weeks.
- Sea buckthorn oil (40-50 ml) is heated to 40 ° C and inserted into the rectum for 20-30 minutes. The course of treatment is 10-15 days. The procedure is best done before bed.
- With a severe pain syndrome, which significantly limits the patient's mobility and worsens his quality of life, microclysters can be used with novocaine. 2 ampoules of a 2% solution of novocaine are dissolved in 180 ml of a steep decoction of chamomile. Hold for at least 50 minutes. Repeat daily for 1 week.
Anti-inflammatory drugs, antiseptics, and antibiotics can also be used from drugs for microclysters. The use of these drugs is allowed strictly in the indicated dosage with the approval of a doctor.
Treatment of chronic prostatitis: step-by-step instructions
The use of various treatment methods is not enough to completely eliminate chronic prostatitis. If a man does not monitor his diet and change his lifestyle, exacerbations regularly occur, which lead to irreversible changes in the structure and functional activity of the prostate, as well as persistent dysuric and sexual disorders. In order to increase the effectiveness of treatment and the duration of remission, you should follow the recommendations in the instructions below for patients with chronic prostatitis.

- Step 1. If a man is diagnosed with chronic prostatitis, he should first adjust his diet. It is necessary to exclude from the menu foods with a large amount of fat, salt and spices. Fats increase blood cholesterol, and salt promotes fluid retention and edema in prostate tissue. Spices (like various chemical additives) irritate the mucous membranes of the urinary tract and exacerbate existing symptoms.
- Step 2. It is also necessary to completely eliminate alcoholic beverages, as they slow down the absorption of nutrients, disrupt blood circulation and lymph, and negatively affect the metabolism in the prostate. If a man suffers from tobacco addiction, measures should be taken to get rid of this habit (toxic substances in tobacco smoke disrupt the viscosity and flowability of prostate secretions, changing their chemical composition).
- Step 3. Overweight men should consult an endocrinologist and nutritionist for a comprehensive diagnosis and correction of body weight, taking into account the deviations found. Obesity is the most important factor in the development of chronic prostatitis, and an important stage in complex therapy is weight loss in patients with a high BMI.
- Step 4. In order to eliminate overload associated with a hypodynamic disorder, an adequate level of physical activity must be provided, commensurate with age and physical fitness. Swimming, physical therapy exercises, stretching exercises, walking are useful for prostatitis.
- Step 5. For the normal functioning of the prostate, it is necessary to monitor the quality of sexual life. It is advisable to have a constant sexual partner, to avoid episodes of sexual arousal when there is no possibility of further intercourse, and to regularly check for genital infections, which can also make chronic prostatitis worse.
Men with recurrent prostatitis need to monitor emotional stress, avoid stressful situations and be exposed to cold or drafts for long periods of time.
Chronic prostatitis is a disease that is difficult to treat, especially if the patient does not follow the prescription of the attending physician and is not responsible about diet and treatment regimen issues. Inflammation of the prostate is dangerous with serious complications, so you need to fully address the problem. Men with this diagnosis should understand that pills alone are not enough to fully restore all functions of the prostate. Therefore, you should not abandon the basic therapy methods recommended by your doctor for chronic prostatitis, even if they cause primary psychological or physical discomfort.

































